Dialysis Access Care
Dialysis Access Procedures
- Vessel Mapping for Access Creation
- Access Evaluation and Treatment of Fistulas and Grafts
- Catheter Procedures
VESSEL MAPPING FOR ACCESS CREATION
 Purpose: to identify the best vessels available for your surgeon to create the best vascular access for you.
Purpose: to identify the best vessels available for your surgeon to create the best vascular access for you.
Whether you’re new to dialysis or have been on dialysis for many years, vessel mapping is essential. For those new to dialysis, vascular mapping gets rid of the guess work, giving your surgeon “the lay of the land,” arming him with the best information possible to create your optimal access. For patients not new to dialysis who are currently experiencing access problems or have been told they have “no vessels” for access creation, a mapping procedure may indicate otherwise. Simply put, if a new access is going to be created for you, the vessels should be imaged prior to surgery.
What You Need to Know
At Open Access, vessel mapping can be performed either through the use of ultrasound, X-ray imaging (venogram) or a combination of the two.
Ultrasound
With ultrasound imaging, a handheld device is passed lightly over the skin above your blood vessels. Sound waves are used to create pictures of your arteries and veins.
Venogram
A venogram involves injecting iodine contrast (X-ray dye) into the veins of the extremity where your access will be placed. The X-ray dye allows the vessels to be imaged and evaluated as needed.
Through the use of ultrasound and/or venography, the Open Access physician will be able to see your vessels, identifying the ideal location for access creation. Normally, patients experience minimal to no discomfort during either of these procedures. The results will be shared with your referring physician.
EVALUATION AND TREATMENT OF DYSFUNCTIONAL FISTULAS AND GRAFTS
 Purpose: to identify and treat problems affecting the functionality of your vascular access.
Purpose: to identify and treat problems affecting the functionality of your vascular access.
What You Need to Know
Unfortunately for most living with grafts and fistulas, minimally invasive procedures are often required to ensure your access is functioning properly. In fact, the average dialysis patient with a graft or fistula requires more than one procedure per year on their access. So if your access is not functioning properly, don’t fret – you are not alone. Whether your access has stopped working completely or it is not functioning as well as it could be, the team at Open Access will do their best to make sure your access works its best.
Your access evaluation will begin with the physician and Open Access care team, looking, listening and feeling your access. Your access will then be imaged with ultrasound, providing the physician with a clearer picture of what is going on. Based on this information, the physician may elect to perform one of the procedures as described below to help restore the functionality of your access.
Fistulogram/Venogram/Arteriogram
Performing these studies will require you to be brought into one of our surgical suites where you will be monitored and cared for before, during and after your procedure. Similar to the venogram performed during vascular mapping, these imaging procedures require injection of iodine contrast (X-ray dye) into your access, arteries and/or veins. By doing so, your Open Access physician will be able gather more detailed information as to why your access is not functioning the way it should be. Once the physician has identified your specific problem, he will likely proceed to fix it using one of the minimally invasive techniques as described below:
Angioplasty/Stenting
Angioplasty and/or stenting is typically performed on areas of stenosis (narrowing) in your arteries or veins. These narrowings can impact how your access functions. They can cause you to have poor dialysis, prolonged bleeding when needles are removed after your treatment, aneurysms (lumps or bumps), swelling of the extremity where your access resides or clotting of your access to name a few. As such, it is important to treat these narrowings to allow for optimal functioning and care of your access.
Angioplasty, also known as balloon dilatation, is typically the first line of treatment for stenosis. It involves inserting a small balloon into your access, artery or vein and inflating the balloon stretching open the narrowed segment. Following a successful angioplasty, the balloon will be deflated and removed.
If the Open Access physician believes the angioplasty was not successful, he may opt to place a stent. A stent is a wire mesh-like tube that can function as a scaffolding placed inside your blood vessel to help keep a narrowed segment open. Whether you require angioplasty and/or stenting, following your procedure you will be discharged by a member of the Open Access team who will answer any of your questions and provide you with detailed instructions for optimal access care along with scheduling your follow-up appointment.
Declotting
If your access has stopped working, you may be referred to us for urgent care. The Open Access physician and care team will evaluate you, explain treatment options, and upon your consent, escort you into one of our surgical suites. The physician will then proceed to remove the clot from your access and perform a fistulagram/venogram/arteriogram to determine why the access stopped working. Often angioplasty and occasionally stenting will be required. Following a successful declotting procedure, you will be able to return to your dialysis unit to receive your next treatment.
CATHETER PROCEDURES
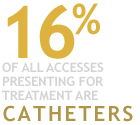 Purpose: to ensure your catheter is placed properly, functioning optimally and removed timely.
Purpose: to ensure your catheter is placed properly, functioning optimally and removed timely.
What You Need to Know
There are four basic types of catheter-related procedures performed at Open Access:
New Catheter Placement
In order to place a new catheter for dialysis, the Open Access physician will evaluation you using ultrasound and or X-ray dye to determine the most appropriate site to have your catheter placed. Using sterile technique, the best catheter will be inserted to allow for optimal dialysis. Sutures will be placed to secure the catheter in place. You will be given instructions prior to discharge from the Open Access care team on how to care for your catheter.
Catheter Declotting
If your catheter is not functioning properly at dialysis, a catheter declotting procedure may be performed at our center. This involves placing clot-dissolving medication in the catheter lumens (tubes). Once this medication has had time to work, you will then be taken into our procedure room where the clot-dissolving medication will be removed and the catheter assessed with regards to how it is now functioning. If your catheter is still not functioning properly, a wire may be placed inside your catheter to clean out the catheter lumen. Your catheter function will be assessed once more and imaging may be performed using X-ray dye if it is still not functioning properly. If after the clot-dissolving medication and guidewire cleaning it is determined that your catheter is now functioning properly, you will return to your dialysis unit to complete your dialysis treatment. You are encouraged to remind your dialysis care team of your recent procedure, as they may want to reduce the amount of Heparine used during your next treatment.
It is important to note that even though your catheter may appear to be functioning properly after your declotting procedure, once back on dialysis, there is always the possibility that your catheter still may not function as desired. If this is the case, your catheter may need to be exchanged for a new one.
Catheter Exchange
Whether your catheter is not functioning properly or your catheter is believed to be infected, your catheter may need to be exchanged. If so, a local anesthetic will be used to numb the tissue around the site where the catheter exits your body. If you desire, IV medication can also be used to allow for greater sedation and pain control.
During the catheter exchange procedure, the blood vessel where the catheter lives will be evaluated using X-ray dye, as sometimes tissue known as “fibrin sheath” can grow around the catheter causing the catheter to malfunction. If this is the reason for your catheter to fail, during the exchange procedure the tissue may be broken apart, typically using an angioplasty balloon. A new catheter will then be inserted through your current catheter track, exiting the body in the same location as the old catheter did. The new catheter will be secured in place with a suture and instructions will be provided to you on how to care for your catheter prior to discharge. You are encouraged to remind your dialysis care team of your recent procedure, as they may want to reduce the amount of Heparine used during your next treatment.
Catheter Removal
Whether the skin overlying and surrounding your catheter is felt to be infected, you have a permanent access (graft or fistula), or you are coming off dialysis, your catheter may need to be removed. For patients with infected catheters with drainage oozing from the exit site, your catheter may need to be removed with a new catheter then placed in a new location. During the catheter removal procedure, local anesthetic will be used to numb the tissue around the site where the catheter exits your body. If you desire, IV medication can be given to allow for greater sedation and pain control. Prior to removing the catheter, the vein where your catheter resides may be imaged using X-ray dye to evaluate for potential abnormalities within the vein that may have occurred as a result of the catheter residing in that vein. If such abnormalities are detected, they may be treated during your catheter removal procedure. Once the catheter is removed, a bandage will be applied. It is advisable not to do any heavy lifting and to refrain from showering/bathing for the next 48 hours. These instructions, and more, will be discussed with you prior to discharge.